Cumulative COVID-19 deaths in India have revealed more than just numbers—they’ve painted a vivid picture of inequality, regional disparities, and systemic challenges. From overwhelmed hospitals to undercounted fatalities, the virus didn’t just affect health—it exposed the cracks in infrastructure, healthcare access, and policy execution across different states.
This article explores the cumulative COVID-19 death toll in India with a focus on regional variation, variant impact, policy response, and underreporting. We dive into how certain states suffered more, the role of variants like Delta and Omicron, and why official data might not reflect the full reality. A clear overview of disparities and their causes gives us a deeper understanding of the pandemic’s true impact on India.
Cumulative COVID-19 Deaths
India’s cumulative COVID-19 deaths have not been evenly spread across its vast geography. While some states managed to control the spread early and limit fatalities, others faced a severe shortage of healthcare resources and suffered higher losses. States like Maharashtra, Delhi, Tamil Nadu, and Uttar Pradesh recorded the highest death tolls. Factors such as population density, urban infrastructure, and the strength of local healthcare systems played a huge role in this uneven outcome.
At the same time, the official numbers have often been questioned due to underreporting, especially in rural regions. Limited testing and inconsistent death certification have led to discrepancies between recorded and estimated deaths. As a result, independent studies and media investigations suggest the real numbers could be significantly higher than reported.
Overview Table: Key Aspects of Cumulative COVID-19 Deaths in India
| Aspect | Details |
| Top Affected States | Maharashtra, Delhi, Tamil Nadu, Uttar Pradesh |
| Major Variants | Delta (most fatal), Omicron (high spread, lower death rate) |
| Challenges | Underreporting, healthcare access, data inconsistency |
| Policy Factors | State-level health responses, lockdown timing, vaccination drives |
| Data Discrepancy | Estimated deaths often double the official count |
| Long-term Effects | Post-COVID health issues contributing to later deaths |
Regional Disparities in Death Toll
India’s federal structure means states handle their own health systems. This led to a wide variation in how the pandemic was managed. While Kerala initially gained praise for early containment, states like Bihar and Uttar Pradesh struggled with resource shortages. Maharashtra and Delhi, with high urban populations, recorded large numbers of cumulative COVID-19 deaths, in part due to higher case numbers and strained hospital systems.
Rural regions were hit hard during the second wave, especially with the Delta variant. Many deaths went unreported due to lack of access to testing and medical care. This uneven spread highlighted how infrastructure and governance directly influenced fatality outcomes.
The Impact of Variants: Delta and Omicron
The Delta variant proved to be the deadliest in India, particularly during the second wave in early 2021. It overwhelmed healthcare systems, with oxygen shortages and mass hospitalizations contributing to a surge in fatalities. Most of the cumulative COVID-19 deaths can be linked to this period.
In contrast, Omicron, which spread rapidly in early 2022, led to a significant rise in cases but far fewer deaths. It exposed vulnerabilities in disease tracking but also showed the benefits of vaccination in reducing mortality. However, the long-term health effects of both variants continue to affect many individuals, contributing to indirect deaths over time.
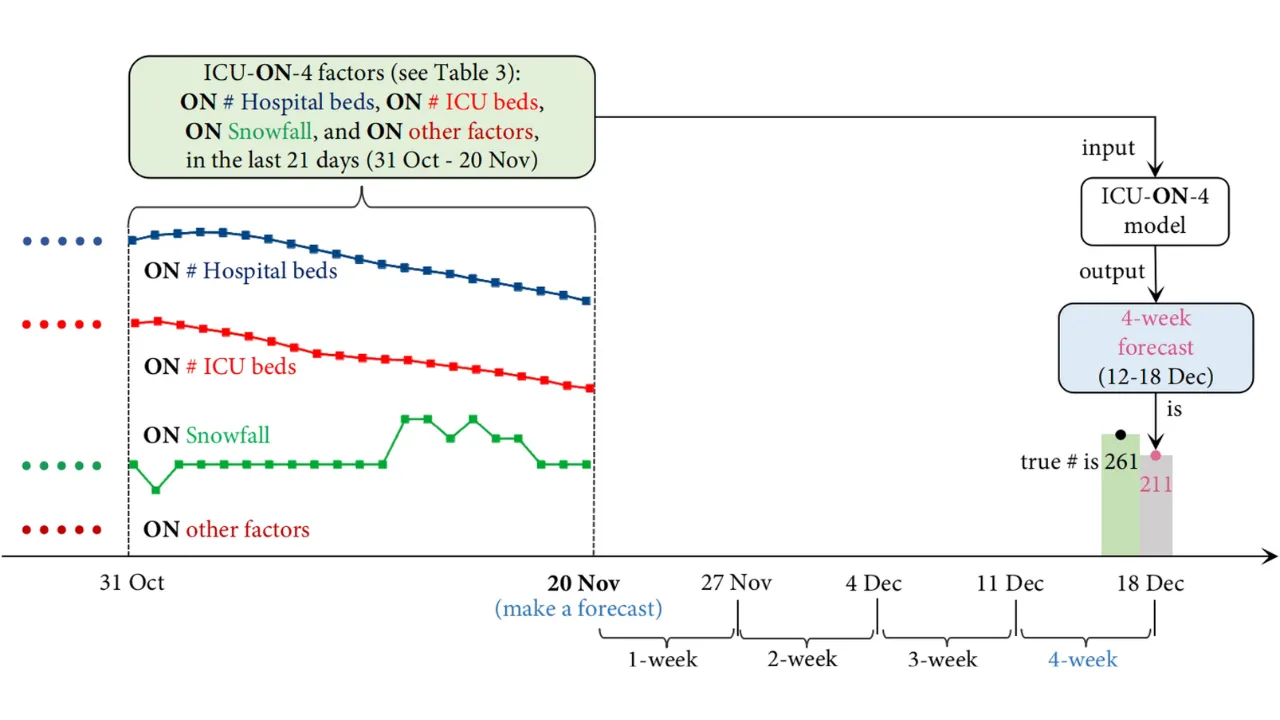
Forecasting and Death Projections
In the early phases of the pandemic, several models attempted to predict India’s COVID-19 death toll. Many projections underestimated the impact, especially during the Delta wave. Retrospective analysis shows that these models failed to account for underreporting, regional disparities, and variant mutations.
Forecasting inaccuracies caused confusion and affected government planning, sometimes leading to delayed responses. These missteps had real consequences on the ground, as seen in cities where health infrastructure collapsed under pressure.
Underreporting and Data Discrepancies
One of the most controversial aspects of cumulative COVID-19 deaths in India is the issue of underreporting. Several independent investigations, including crematorium and burial ground data, suggested that the actual death toll could be two to three times higher than the official count.
Underreporting was particularly severe in rural and semi-urban areas. The reasons included lack of medical certification, stigma around COVID-19, and political pressure to keep numbers low. These discrepancies have led to mistrust in official data and demand for more transparency in future health crises.
Policy Response and Healthcare Systems
The effectiveness of public health policies varied across states. Some, like Kerala and Tamil Nadu, implemented strict early lockdowns and invested in testing and contact tracing. Others, especially those with weaker health systems, were slower to act and struggled with logistics.
Vaccination rollout also varied, affecting mortality outcomes. States with higher vaccination rates saw fewer deaths during the Omicron wave. This shows that coordinated policy, proper funding, and timely decision-making were essential to controlling the fatality rate.
List: Key Factors Influencing Cumulative COVID-19 Deaths
- Healthcare Infrastructure
- States with better hospital facilities, ICU beds, and oxygen supply recorded fewer preventable deaths.
- States with better hospital facilities, ICU beds, and oxygen supply recorded fewer preventable deaths.
- State-level Policy
- Strict lockdowns, effective testing strategies, and early vaccine rollout reduced mortality in several regions.
- Strict lockdowns, effective testing strategies, and early vaccine rollout reduced mortality in several regions.
Socioeconomic Disparities and Mortality
The burden of cumulative COVID-19 deaths was heavier on marginalized communities. Low-income populations had limited access to healthcare, less ability to socially distance, and often lived in high-density housing. Migrant workers faced severe challenges, including job loss and lack of transportation, which contributed to indirect deaths and worsening health outcomes.
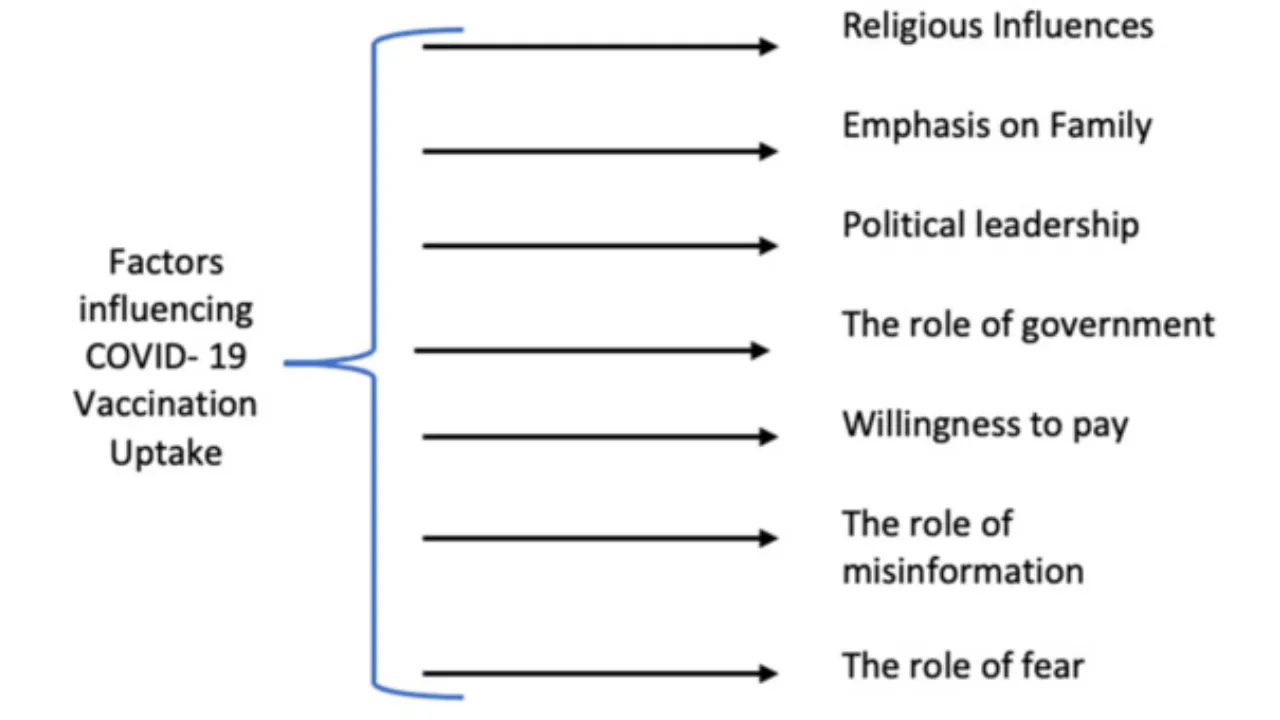
Socioeconomic status also affected vaccine access and awareness. In regions where education and health literacy were lower, misinformation led to vaccine hesitancy and delayed care-seeking behavior, increasing the death toll.
Long-Term Mortality Effects
Even after the peak of the pandemic, India continues to experience deaths linked to COVID-19 complications. Long COVID, weakened immunity, and delays in treatment for other conditions during the pandemic have all contributed to ongoing fatalities. The cumulative COVID-19 deaths must also account for these delayed impacts, which are harder to track but equally significant.
FAQs
1. Why are cumulative COVID-19 deaths higher in some Indian states?
Some states had better health infrastructure and quicker responses, while others lacked resources, leading to higher fatalities.
2. How accurate are India’s official COVID-19 death numbers?
Many believe they are underreported. Independent estimates suggest the real numbers could be much higher.
Final Thought
India’s cumulative COVID-19 deaths tell a complex story of regional challenges, policy gaps, and a healthcare system pushed to its limits. Understanding this data helps us prepare better for the future. If this topic interests you, share your thoughts in the comments or explore related content like how your state responded or your personal COVID-19 horoscope to reflect on the pandemic’s effect in your life.